Imagine your heart racing unexpectedly or feeling a flutter in your chest. These sensations could be signs of atrial fibrillation, commonly known as AFib. AFib is a serious heart condition that affects millions worldwide, yet many people remain unaware of its implications and symptoms.
In this article, you’ll discover what AFib really is, how it disrupts the normal rhythm of your heart, and why understanding it matters for your health. From recognizing the warning signs to exploring treatment options, we’ll guide you through everything you need to know about this prevalent condition. Are you ready to take control of your heart health? Let’s dive deeper into the world of AFib and uncover the vital information that could change your life.
What Is Afib?
Atrial fibrillation, commonly known as AFib, is a heart condition characterized by an irregular and often rapid heartbeat. It occurs when the heart’s two upper chambers (the atria) experience chaotic electrical signals. This disruption can lead to various symptoms and complications.
AFib may manifest through several noticeable signs:
- Palpitations: You might feel your heart racing or fluttering.
- Shortness of breath: Even with mild exertion, you could struggle to catch your breath.
- Fatigue: Sudden tiredness may occur without any apparent reason.
- Dizziness or lightheadedness: You may experience feelings of faintness or vertigo.
The implications of AFib extend beyond discomfort. This condition increases the risk of stroke, heart failure, and other serious cardiovascular issues. In fact, people with AFib are five times more likely to have a stroke compared to those without it.
Understanding the types of AFib can also be helpful:
- Paroxysmal AFib: Episodes come and go spontaneously; they usually last less than a week.
- Persistent AFib: Episodes last longer than seven days and require medical intervention for restoration of normal rhythm.
- Permanent AFib: The condition is ongoing; doctors focus on managing symptoms rather than restoring normal rhythm.
It’s essential to recognize these aspects of AFib for timely diagnosis and treatment. Awareness helps in taking proactive steps towards better heart health.
Symptoms of Afib
Atrial fibrillation (AFib) often presents several noticeable symptoms. Recognizing these signs is crucial for timely intervention and management.
Common Symptoms
- Racing heart: You might feel your heart racing or pounding, indicating irregular heartbeats.
- Chest fluttering: Some experience a sensation of fluttering in the chest, which can be alarming.
- Shortness of breath: Difficulty breathing during routine activities or even at rest may occur.
- Fatigue: Unusual tiredness can happen, making daily tasks more challenging.
- Dizziness or lightheadedness: A sense of dizziness can lead to a risk of fainting.
These symptoms vary among individuals, so it’s important to note any changes in your body’s signals.
Potential Complications
If left unmanaged, AFib can lead to serious complications. Understanding these risks helps you stay informed:
- Stroke: Blood clots can form due to stagnant blood in the heart’s chambers, increasing stroke risk significantly.
- Heart failure: The heart may weaken over time from persistent AFib, leading to heart failure.
- Other arrhythmias: AFib can cause other abnormal heart rhythms that complicate treatment options.
Awareness of these potential complications empowers you to seek medical advice promptly if symptoms arise.
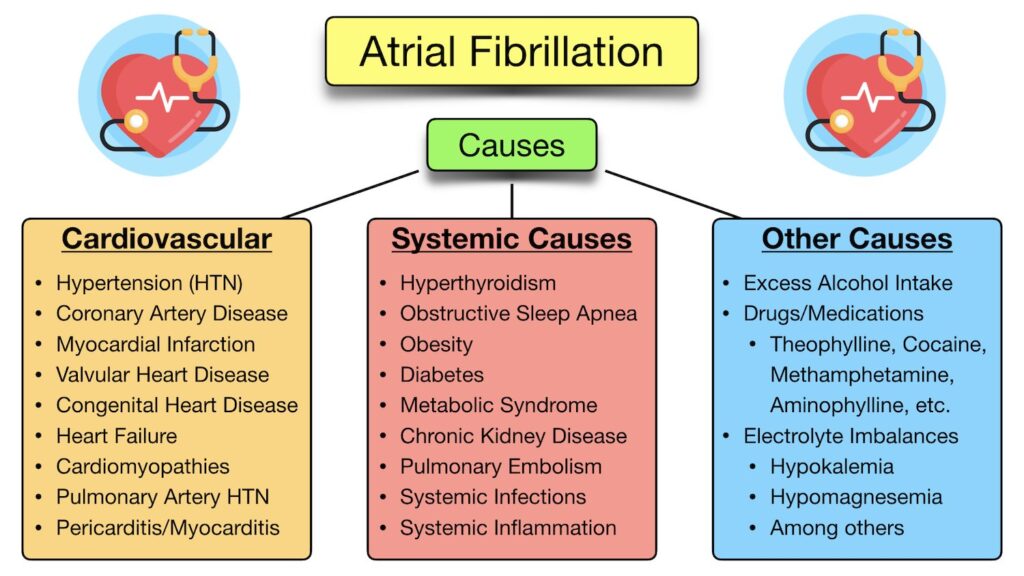
Causes of Afib
Atrial fibrillation (AFib) can arise from various causes, including underlying health conditions and lifestyle factors. Understanding these causes helps in identifying risks and managing your heart health effectively.
Risk Factors
Several risk factors contribute to the likelihood of developing AFib:
- Age: Individuals aged 65 and older face a higher risk.
- Heart disease: Existing conditions like coronary artery disease increase susceptibility.
- High blood pressure: Hypertension strains the heart, promoting AFib development.
- Obesity: Excess weight puts additional stress on the cardiovascular system.
- Diabetes: This condition elevates the risk of developing AFib due to associated heart complications.
Triggers
Certain triggers can provoke or worsen episodes of AFib:
- Alcohol consumption: Even moderate drinking can trigger irregular heartbeats for some people.
- Caffeine intake: For others, excessive caffeine may lead to AFib episodes.
- Stress and anxiety: Emotional stressors can disrupt normal heart rhythms.
- Sleep apnea: Poor sleep quality significantly increases the chances of AFib occurring.
- Illness or infection: Infections that cause fever can also trigger arrhythmias.
Recognizing both risk factors and triggers empowers you to take proactive steps in managing your heart health.
Diagnosis of Afib
Diagnosing atrial fibrillation (AFib) involves a combination of medical history, physical examinations, and specific tests. Early detection plays a crucial role in effective management.
Testing Methods
You might undergo several testing methods to confirm AFib. Common approaches include:
- Electrocardiogram (ECG): This test records the heart’s electrical activity, detecting irregularities in heartbeat patterns.
- Holter Monitor: A portable ECG device worn for 24 to 48 hours captures heart rhythms during daily activities.
- Event Monitor: Similar to a Holter monitor but used over weeks or months, it activates when you feel symptoms.
- Echocardiogram: This ultrasound test visualizes the heart’s structure and function, identifying underlying conditions contributing to AFib.
Interpreting Results
Understanding your test results is vital for managing AFib. Key points include:
- An ECG showing irregular waves indicates potential AFib presence.
- A Holter Monitor may reveal episodes that occur sporadically throughout the day or night.
- An Echocardiogram provides insights into heart size and function; abnormalities can inform treatment options.
Discussing these results with your healthcare provider helps clarify their implications and guide treatment decisions effectively.
Treatment Options for Afib
Managing atrial fibrillation (AFib) involves various treatment options tailored to individual needs. These methods aim to control heart rate, restore normal rhythm, prevent complications, and improve overall heart health.
Medications
Medications are a common first step in treating AFib. They help manage symptoms and reduce the risk of blood clots. Common types include:
- Rate control medications: Beta-blockers like metoprolol and calcium channel blockers such as diltiazem help slow down your heart rate.
- Rhythm control medications: Antiarrhythmic drugs like amiodarone or sotalol may help restore a regular heartbeat.
- Anticoagulants: Blood thinners such as warfarin or newer agents like apixaban can lower stroke risk by preventing clot formation.
These medications require regular monitoring to ensure effectiveness and safety.
Lifestyle Changes
Lifestyle changes play a crucial role in managing AFib effectively. Consider incorporating these modifications into your routine:
- Maintain a healthy weight: Aim for a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting processed foods.
- Limit alcohol intake: Reducing alcohol consumption can decrease triggers for AFib episodes.
- Exercise regularly: Engage in moderate physical activity for at least 150 minutes per week to support cardiovascular health.
- Manage stress levels: Techniques like yoga and meditation can help reduce anxiety that may provoke AFib.
Making these changes can significantly enhance your quality of life.
Surgical Procedures
For some individuals with persistent or severe AFib who don’t respond well to medication, surgical procedures might be necessary. Here are common options:
- Catheter ablation: This minimally invasive procedure targets specific areas of the heart responsible for irregular signals using radiofrequency energy.
- Maze procedure: In this surgery, surgeons create scar tissue within the heart’s upper chambers to disrupt abnormal electrical pathways.
- Left atrial appendage closure (LAAC): This technique reduces stroke risk by sealing off the left atrial appendage where blood clots often form.
These procedures typically require thorough discussions with healthcare providers about benefits and risks.